Home » Supported Research » Multimodal mapping of subcortical and cortical functional network disturbances in focal epilepsy
Multimodal mapping of subcortical and cortical functional network disturbances in focal epilepsy
Title: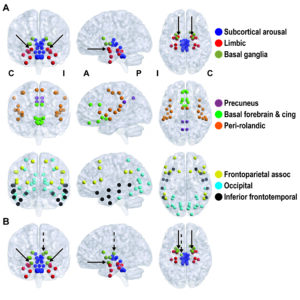
Multimodal mapping of subcortical and cortical functional network disturbances in focal epilepsy
Project Number:
5R00NS097618-05
Contact PI/Project Lead:
Dario Englot
Award Organization:
National Institutes of Health
Abstract:
Epilepsy affects 1% of the population, leading to significant morbidity and mortality. In focal epilepsy, seizures originate from an epileptogenic zone (EZ), and surgical resection leads to seizure-freedom in many patients. However, deleterious effects of focal epilepsy extend beyond the anatomic EZ, including diffuse gray matter atrophy, neocortical hypometabolism, and impaired neurocognitive function. Previous interictal (between seizures) magnetoencephalography studies of functional connectivity in focal epilepsy patients have demonstrated decreased connectivity in association neocortex that is directly related to frequency of consciousness-impairing (but not consciousness-sparing) seizures. Furthermore, prior ictal (during seizures) electrocorticography (ECoG) studies have demonstrated depressed neocortical activity during consciousness-impairing (but not consciousness-sparing) seizures in focal epilepsy. The central hypothesis of the present proposal is that over time, recurrent seizures in focal epilepsy lead to aberrant connections between subcortical activating structures (e.g., thalamus, basal forebrain) and association cortex, resulting in depressed neocortical connectivity that may contribute to neurocognitive dysfunction. To address this hypothesis, the present studies will use functional magnetic resonance imaging (fMRI) to measure interictal functional connectivity between subcortical activating structures and association neocortex in pre-operative focal epilepsy patients vs. controls (Aim 1). Connectivity patterns will be related to seizure type/frequency and neurocognitive parameters. To determine if functional connectivity perturbations are reversible once patients achieve seizure freedom after surgery, fMRI analyses of subcortical-cortical connectivity and neuropsychological tests will be repeated in patients ≥ 1 year post-operatively (Aim 2). Finally, to determine whether abnormal neocortical rhythms during consciousness-impairing seizures (ictal) lead directly to long-term reductions in neocortical connectivity (interictal), dynamic changes in connectivity will be measured before, during, and after seizures using ECoG (Aim 3). It is anticipated that compared to non-epileptic controls, focal epilepsy patients will exhibit reduced subcortical-cortical connectivity on interictal fMRI, which will be related to frequency of consciousness-impairing seizures and neurocognitive dysfunction (Aim 1). However, it is expected that subcortical-cortical functional connectivity perturbations will improve in patients who become seizure free after epilepsy surgery (Aim 2). Finally, it is anticipated that ECoG studies of dynamic functional connectivity will demonstrate ictal reductions in neocortical connectivity during consciousness-impairing seizures compared to baseline, suggesting a direct link between seizure activity and altered neocortical connectivity (Aim 3). A detailed understanding of subcortical-cortical network dysfunction in focal epilepsy gained through these studies may lead to novel targets for neuromodulation-based treatment, improvements in surgical patient selection and outcome prediction, and better strategies to prevent neurocognitive sequelae in this devastating disorder.