Intraoperative Parathyroid Gland Detection and Assessment
Parathyroid Gland Detection
 Endocrine surgery traditionally involves meticulous dissection and resection of diseased glands while leaving the normal glands intact, guided only by visual recognition. Inadvertent removal of parathyroid glands is a recognized complication of this procedure leading to complications such as postoperative hypocalcemia and hypoparathyroidism that could have consequences on the long-term regulation of calcium homeostasis post-operatively. There is a need for an identification tool that provides sensitive, real-time detection of parathyroid glands during surgery. Optical spectroscopy and imaging are powerful tools that can aid in the detection of tissue physiology and pathology. Preliminary fiber probe and imaging measurements have shown that the parathyroid exhibits higher levels of near-infrared (NIR) autofluorescence in comparison to all other tissues in the neck. The main objective of this project then is to develop a technique based on NIR autofluorescence that enables intraoperative detection of parathyroid glands such that accidental removal is minimized by supplementing the standards of visual
inspection.
Endocrine surgery traditionally involves meticulous dissection and resection of diseased glands while leaving the normal glands intact, guided only by visual recognition. Inadvertent removal of parathyroid glands is a recognized complication of this procedure leading to complications such as postoperative hypocalcemia and hypoparathyroidism that could have consequences on the long-term regulation of calcium homeostasis post-operatively. There is a need for an identification tool that provides sensitive, real-time detection of parathyroid glands during surgery. Optical spectroscopy and imaging are powerful tools that can aid in the detection of tissue physiology and pathology. Preliminary fiber probe and imaging measurements have shown that the parathyroid exhibits higher levels of near-infrared (NIR) autofluorescence in comparison to all other tissues in the neck. The main objective of this project then is to develop a technique based on NIR autofluorescence that enables intraoperative detection of parathyroid glands such that accidental removal is minimized by supplementing the standards of visual
inspection.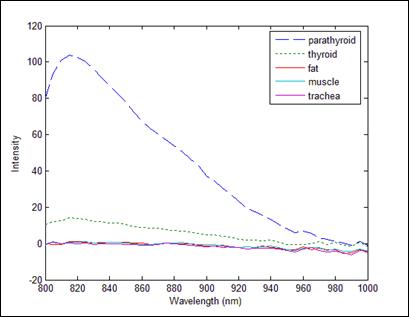 Aspects of the project include: (1) characterizing the NIR fluorescence signatures of parathyroid and thyroid tissues, (2) studying the basis of the observed differences in the spectral characteristics, (3) developing a software interface and automating data acquisition and along with a next-generation clinical system, (4) collecting a large patient database and performing retrospective and prospective evaluation discrimination algorithms and studying the effect of the disease state on spectral measurements and (5) assessing lymph nodes for the presence of thyroid or parathyroid cancer. The results of the proposed work will have a significant impact on health care by providing guidance towards dissection and resection of thyroid and parathyroid tissues. This would potentially result in fewer complications due to accidental injury or incomplete removal of parathyroid tissue.
Aspects of the project include: (1) characterizing the NIR fluorescence signatures of parathyroid and thyroid tissues, (2) studying the basis of the observed differences in the spectral characteristics, (3) developing a software interface and automating data acquisition and along with a next-generation clinical system, (4) collecting a large patient database and performing retrospective and prospective evaluation discrimination algorithms and studying the effect of the disease state on spectral measurements and (5) assessing lymph nodes for the presence of thyroid or parathyroid cancer. The results of the proposed work will have a significant impact on health care by providing guidance towards dissection and resection of thyroid and parathyroid tissues. This would potentially result in fewer complications due to accidental injury or incomplete removal of parathyroid tissue. Researchers
Faculty
Post Doctoral Scholars and Graduate Students
- Giju Thomas
- Parker Willmon
Collaborators
- Carmen C. Solorzano, Vanderbilt University Medical Center
- Naira Baregamian, Vanderbilt University Medical Center
Publications
Thomas, G. et al. Innovative surgical guidance for label-free real-time parathyroid identification. Surgery 165, 114–123 (2019).
Thomas, G. et al. Developing a Clinical Prototype to Guide Surgeons for Intraoperative Label-Free Identification of Parathyroid Glands in Real Time. Thyroid 28, 1517–1531 (2018).
McWade, M. A., Sanders, M. E., Broome, J. T., Solórzano, C. C. & Mahadevan-Jansen, A. Establishing the clinical utility of autofluorescence spectroscopy for parathyroid detection. Surgery 159, 193–202 (2016).
McWade, M. A. et al. Label-free Intraoperative Parathyroid Localization With Near-Infrared Autofluorescence Imaging. J. Clin. Endocrinol. Metab. 99, 4574–4580 (2014).
McWade, M. A. et al. A novel optical approach to intraoperative detection of parathyroid glands. Surgery 154, 1371–7; discussion 1377 (2013).
Paras, C., Keller, M., White, L., Phay, J. & Mahadevan-Jansen, A. Near-infrared autofluorescence for the detection of parathyroid glands. J. Biomed. Opt. 16, 067012 (2011).
Assessment of Parathyroid Viability
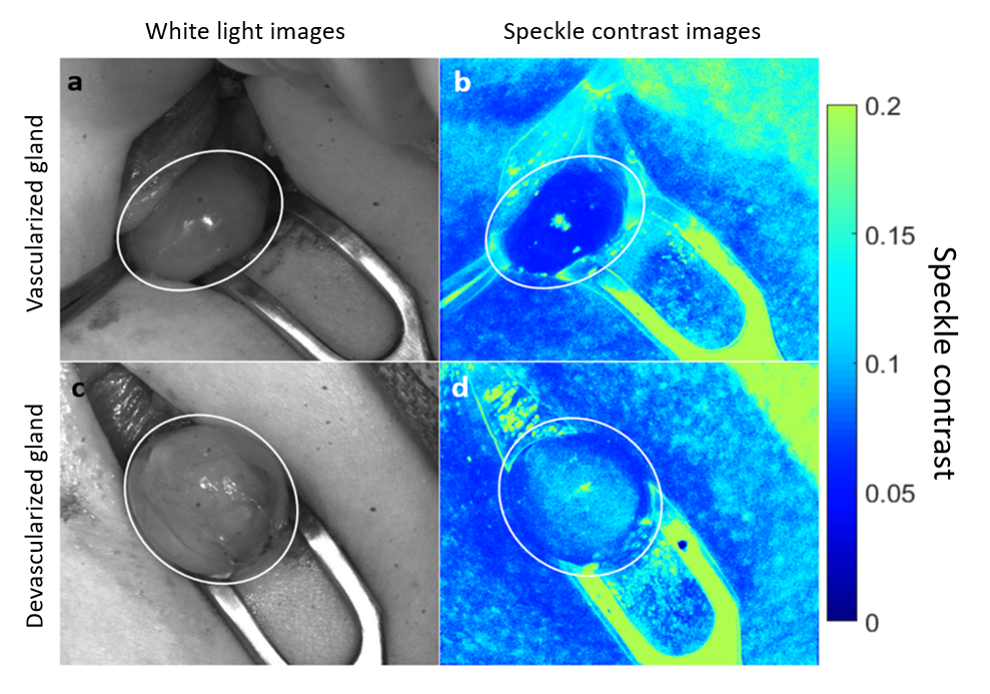 Post-surgical hypoparathyroidism and hypocalcemia are known to occur after nearly 50% of all thyroid surgeries as a result of accidental disruption of blood supply to healthy parathyroid glands. These glands are responsible for regulating blood calcium and so damage to them leads to dire consequences like muscle spasms, cardiac arrhythmia and tetany. However, there are currently no clinical methods for accurately identifying compromised glands and the surgeon relies on visual assessment alone to determine if any gland(s) should be excised and auto-transplanted to salvage its function. Laser Speckle Contrast Imaging (LSCI) enables real-time assessment of parathyroid viability and we have shown that it is capable of distinguishing between well-vascularized and compromised parathyroid glands during thyroid surgery with an accuracy of 91.5%. It is also capable of detecting parathyroid gland vascular compromise when it may not be visually apparent to the surgeon. Measurements can be performed in real-time and without the need to turn off operating room lights. LSCI shows promise as a real-time, contrast-free, objective method for helping reduce hypoparathyroidism after thyroid surgery.
Post-surgical hypoparathyroidism and hypocalcemia are known to occur after nearly 50% of all thyroid surgeries as a result of accidental disruption of blood supply to healthy parathyroid glands. These glands are responsible for regulating blood calcium and so damage to them leads to dire consequences like muscle spasms, cardiac arrhythmia and tetany. However, there are currently no clinical methods for accurately identifying compromised glands and the surgeon relies on visual assessment alone to determine if any gland(s) should be excised and auto-transplanted to salvage its function. Laser Speckle Contrast Imaging (LSCI) enables real-time assessment of parathyroid viability and we have shown that it is capable of distinguishing between well-vascularized and compromised parathyroid glands during thyroid surgery with an accuracy of 91.5%. It is also capable of detecting parathyroid gland vascular compromise when it may not be visually apparent to the surgeon. Measurements can be performed in real-time and without the need to turn off operating room lights. LSCI shows promise as a real-time, contrast-free, objective method for helping reduce hypoparathyroidism after thyroid surgery.
Researchers
Faculty
Post Doctoral Scholars and Graduate Students
- Giju Thomas
- Han Dong
Collaborators
- Carmen C. Solorzano, Vanderbilt University Medical Center
- Naira Baregamian, Vanderbilt University Medical Center
Publications
Mannoh, E. A., Thomas, G., Solórzano, C. C. & Mahadevan-Jansen, A. Intraoperative Assessment of Parathyroid Viability using Laser Speckle Contrast Imaging. Sci. Rep. 7, 14798 (2017).