Kulapatana, Surat; Okamoto, Luis E.; Rigo, Stefano; Urechie, Vasile; Cayton, Thomas W.; Han, Ruijing E.; Jacob, Giris; Dupont, William D.; Furlan, Raffaello; Biaggioni, Italo O.; & Diedrich, André M. (2026). Hyperadrenergic postural tachycardia syndrome associated with augmented neurovascular transduction. Clinical Autonomic Research. https://doi.org/10.1007/s10286-025-01183-z
Muscle sympathetic nerve activity, or MSNA, is important for understanding postural tachycardia syndrome (POTS), but directly measuring it using microneurography is not practical in a clinical setting. In this study, we evaluated whether the rise in diastolic blood pressure during phase 2 of the Valsalva maneuver, called DBPVM2l_rise, could serve as a simpler marker of sympathetic activity. We also explored enhanced neurovascular transduction as a potential mechanism in hyperadrenergic POTS.
We studied 21 women with POTS and 22 healthy women using Valsalva maneuvers and microneurography. MSNA spike rates were analyzed using a specialized wavelet method. The DBPVM2l_rise cutoff for hyperadrenergic POTS was determined by optimizing its correlation with MSNA measurements. We also defined peripheral sympathetic neurovascular transduction (psNVT) as the ratio of DBPVM2l_rise to the early phase 2 MSNA increase and compared responses between hyperadrenergic and non-hyperadrenergic patients.
In healthy participants, DBPVM2l_rise was strongly correlated with the percentage change in phase 2 MSNA spike rate. A cutoff of 15 mmHg effectively separated POTS patients into hyperadrenergic (DBPVM2l_rise ≥ 15 mmHg) and non-hyperadrenergic (DBPVM2l_rise < 15 mmHg) groups. While both groups had similar MSNA spike rates, hyperadrenergic patients had higher baseline systolic blood pressure, faster pressure recovery, and greater psNVT, indicating enhanced neurovascular responsiveness.
These findings suggest that a DBPVM2l_rise of 15 mmHg or higher could serve as a practical clinical marker for hyperadrenergic POTS. Patients with hyperadrenergic POTS show heightened neurovascular responses despite having similar MSNA levels, emphasizing the value of sympathetic markers in guiding clinical assessment and management.
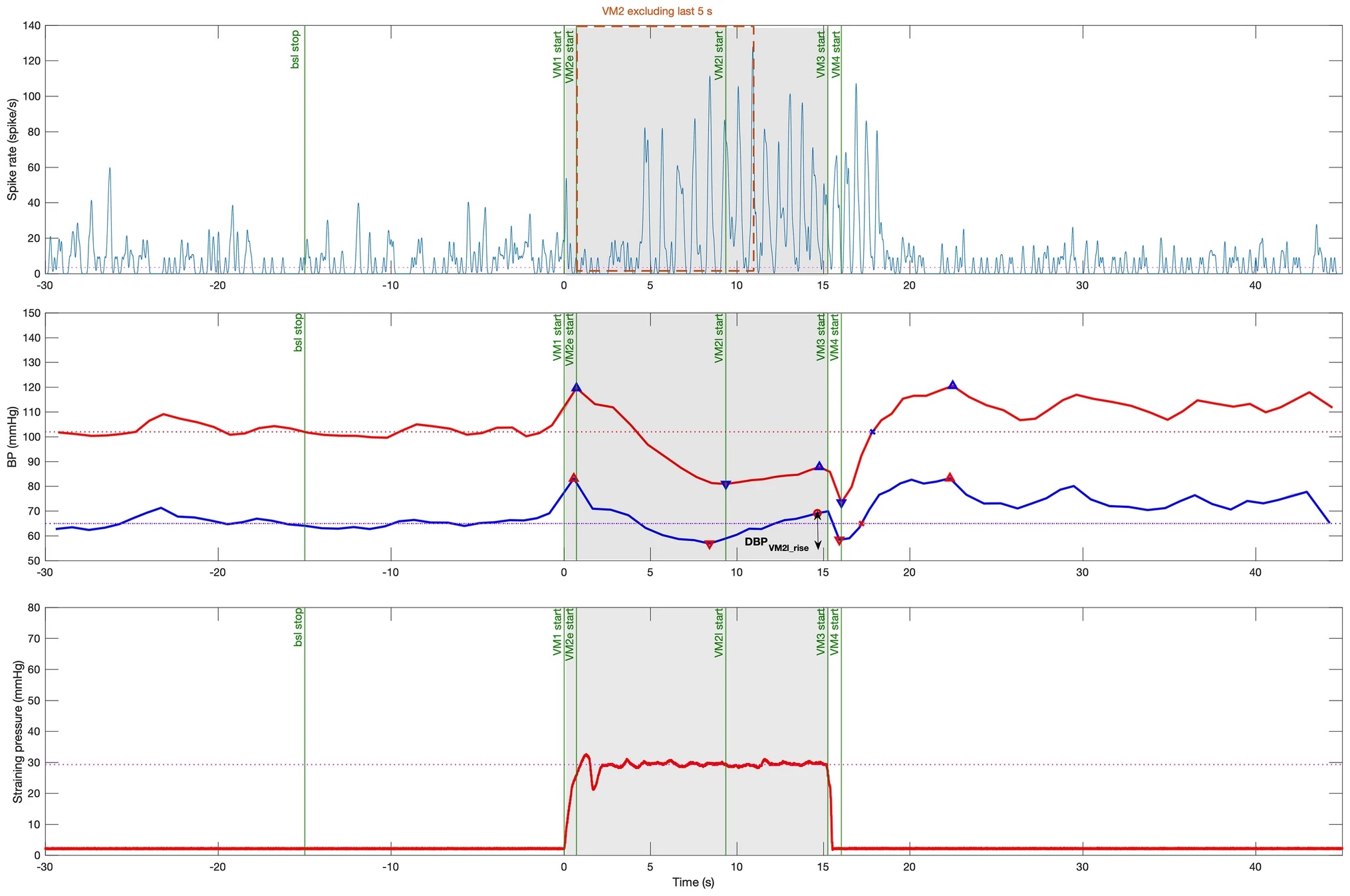
Fig 1
Example recording of a healthy subject performing a 30-mmHg Valsalva maneuver. Valsalva phases were defined based on straining time and blood pressure changes (green vertical lines). Bsl baseline, VM1 Valsalva phase 1, VM2e early Valsalva phase 2, VM2l late Valsalva phase 2, VM3 Valsalva phase 3, VM4Valsalva phase 4. Top panel: continuous MSNA spike rate smoothed by a 3-Hz cutoff frequency Gaussian filter. The orange box represents MSNA spike rate in phase 2 excluding the last 5 s. Middle panel: continuous finger systolic blood pressure (SBP, red) and diastolic blood pressure (DBP, blue). Horizontal lines represent baseline blood pressures. The late phase 2 DBP rise (DBPVM2l_rise) is the difference between the VM2 DBP nadir and the subsequent maximum at the end of VM2 (vertical line with arrows). Bottom panel: Valsalva straining pressure. The subject was asked to hold pressure at 30 mmHg for 15 s (gray area)