Kawel-Boehm, N., Hansen, S. L., Ambale-Venkatesh, B., Carr, J. J., Finn, J. P., Jerosch-Herold, M., Kawut, S. M., McClelland, R. L., Post, W. S., Prince, M. R., Shea, S. M., Lima, J. A. C., & Bluemke, D. A. (2025). Validation of normal reference ranges in cardiac magnetic resonance imaging: The Multi-Ethnic Study of Atherosclerosis. Journal of Cardiovascular Magnetic Resonance, 27(2), 101949. https://doi.org/10.1016/j.jocmr.2025.101949
In heart imaging studies, “normal” values are usually defined using a simple statistical rule: the average value from a healthy group, plus or minus two standard deviations (the “2-SD method”). This approach is widely used in cardiac magnetic resonance (CMR) imaging, but it has not been well tested to see whether values outside these ranges actually predict future heart problems. The goal of this study was to evaluate whether commonly used CMR reference ranges are clinically meaningful—that is, whether they are linked to later cardiovascular (CV) events.
Researchers first established normal reference ranges for measurements of the left and right sides of the heart using CMR data from 1,518 healthy adults in the Multi-Ethnic Study of Atherosclerosis (MESA) who had no known cardiovascular disease or risk factors. These measurements included heart chamber volumes, heart muscle mass, wall thickness, and pumping function (ejection fraction), adjusted for body size. Cut-off values at 1 and 2 standard deviations from the mean were defined. The investigators then examined whether people in the full MESA cohort with CMR data (4,915 participants, including those with CV risk factors) who had values outside these ranges were more likely to experience cardiovascular events over 5 and 10 years of follow-up.
The results showed that several left-ventricular (LV) measurements—such as larger chamber volumes and reduced pumping function—above or below the 2-SD threshold were linked to a higher risk of major and overall cardiovascular events in both men and women. In men, increases in LV muscle mass and wall thickness even beyond the 1-SD threshold were associated with higher risk, while in women, thicker LV walls at 1 SD and higher LV muscle mass at 2 SD were linked to adverse outcomes. In contrast, several right-ventricular measurements and LV end-diastolic diameter were not associated with future cardiovascular events. Similar patterns were seen when outcomes were assessed over 10 years.
Overall, this study supports the clinical usefulness of standard CMR reference ranges for many left-ventricular measurements. Values outside the commonly used “normal” range, especially beyond the 2-SD threshold, were meaningfully associated with increased cardiovascular risk, whereas some other commonly measured parameters were not predictive of future events.
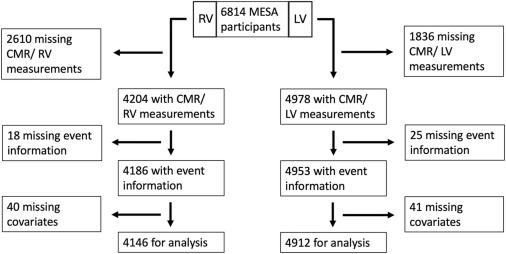
Fig. 1. Study participant flow chart. MESA multi-ethnic study in atherosclerosis, CMR cardiovascular magnetic resonance, LV left ventricle, RV right ventricle