Winkler, Kailey; McKinney, Jared; Reale, Carrie; Anders, Shilo; Rubenstein, Melissa; Cavagnini, Lauren; Crowe, Remle; Ward, Michael J. “A Qualitative Analysis of Barriers to Evidence-Based Care in the Prehospital Management of Patients with Suspected Acute Coronary Syndrome.” Prehospital Emergency Care 29, no. 3 (2025): 274-282. https://doi.org/10.1080/10903127.2024.2372817.
Prehospital electrocardiograms (ECGs) and giving aspirin are proven methods to help patients with heart conditions like acute coronary syndrome (ACS) before they reach the hospital. However, emergency medical services (EMS) don’t always follow these practices consistently. We wanted to understand what stops EMS from using ECGs and giving aspirin to patients who might have ACS.
In this study, we spoke with EMS workers from three different regions in the U.S. We interviewed paramedics and other staff to find out what challenges they face when providing care to patients suspected of having ACS. We analyzed these interviews using a well-known method to identify common themes.
A total of 25 paramedics and 20 other staff members participated, with an average age of 41, and about 30% of them were women. We found several key issues that affected how care was provided. Before EMS arrived at the scene, things like staffing problems, training, and how calls were assigned affected the diagnosis. During diagnosis and treatment, safety concerns and communication problems sometimes took priority over actually giving care. EMS staff also had to decide how to use their resources, such as whether to send a more advanced team or not. Experienced EMS workers relied on their past experience, while newer workers were guided by their recent training. Uncertainty about the diagnosis, especially when patients had unusual symptoms, also led to mistakes. Once on the way to the hospital, the limitations of EMS workers’ training and resources made it harder to use and interpret ECGs. However, those who used ECGs more often felt they could make quicker decisions. Finally, EMS workers reported that the emotional toll of their work led to stress, bad habits, and burnout. They said they wanted more feedback on their performance, but felt the feedback they got was rare and mostly focused on mistakes.
In conclusion, there are many factors that make it difficult for EMS workers to deliver the best care for ACS patients before they reach the hospital. Better education in interpreting ECGs, more support for decision-making, reducing bias, and providing more useful feedback could help overcome these barriers.
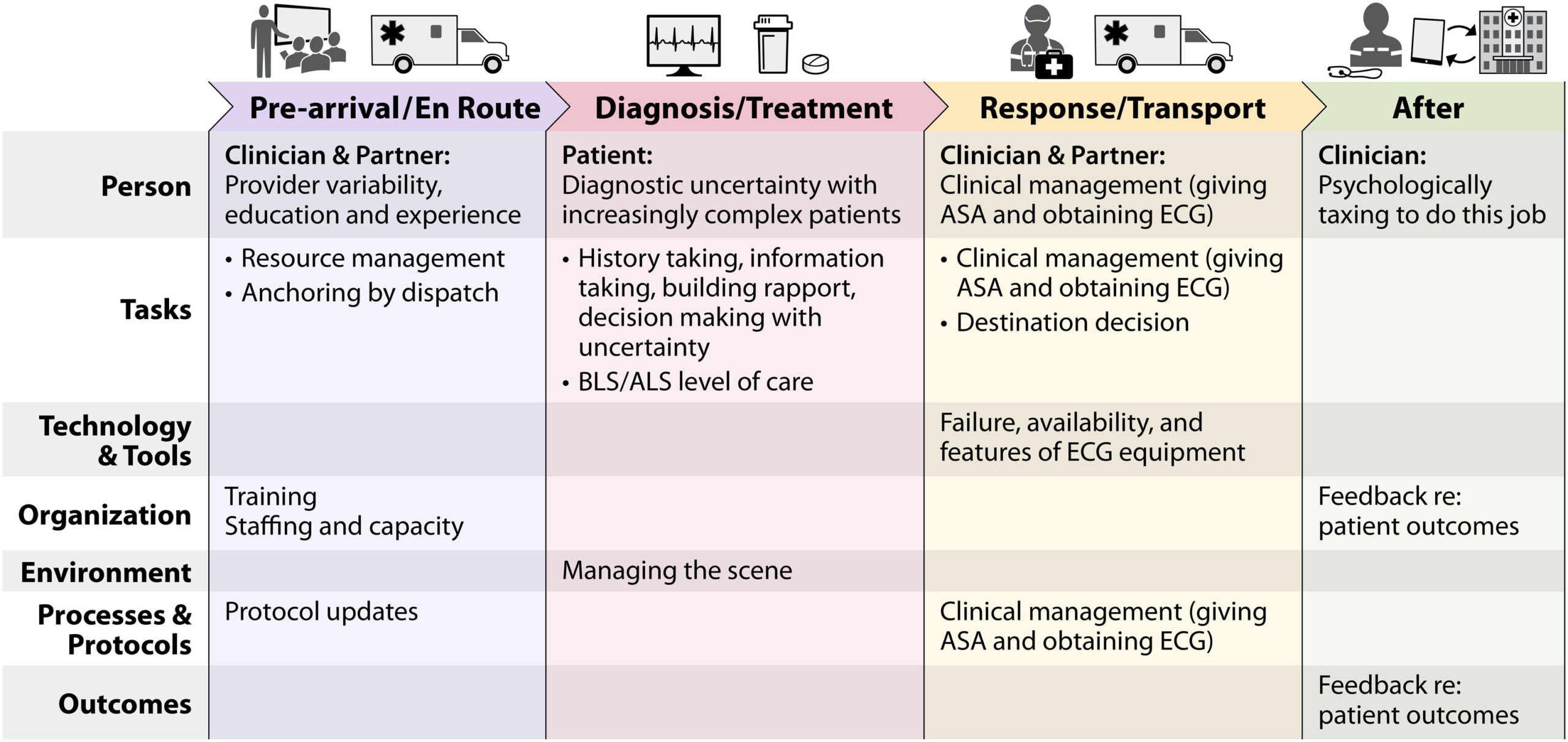
Figure 1.
Summary of themes and subthemes from 45 interviews with EMS clinicians and stakeholders organized by phase of the EMS call (x-axis) and the SEIPS framework domains (y-axis).