Measles
Get the facts about measles, how it spreads, its symptoms, and how vaccination can protect you and your community.
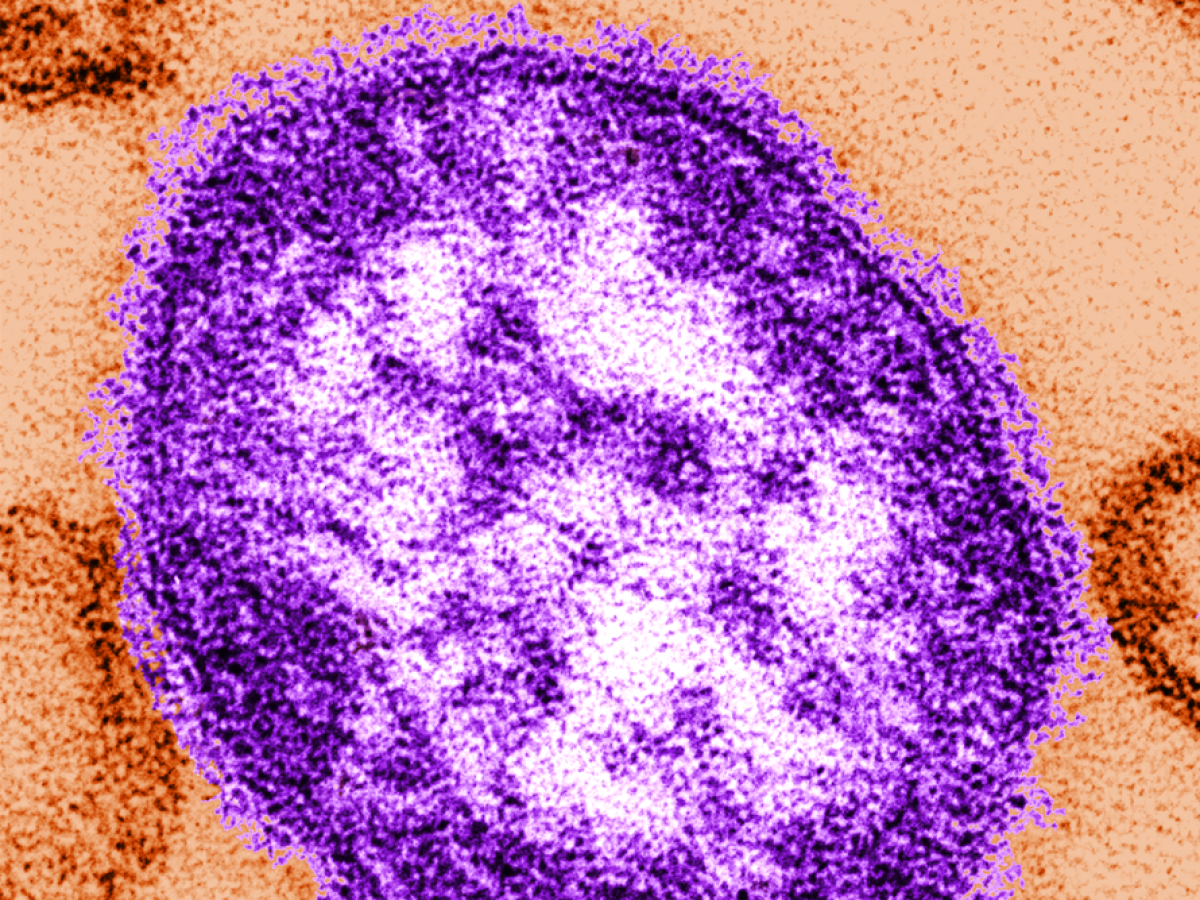
Measles, also known as Rubeola, is a highly contagious virus that spreads through respiratory droplets when an infected person breathes, coughs, or sneezes. Measles can lead to serious complications, including pneumonia, encephalitis, and death, especially in young children and immunocompromised individuals. Vaccination with the MMR (measles, mumps, and rubella) vaccine is the best prevention.
With a 99% vaccination rate among VU students, the risk of transmission within our campus community remains low.
Symptoms
The measles virus progresses through three distinct phases:
Incubation Period:
The incubation period is typically 11-12 days from the time a person is exposed to the virus until their first symptom appears.
Prodromal Phase (Early Symptoms)
- Fever
- Cough
- Runny nose
- Red, watery eyes
- Tiny white spots (Koplik spots) may appear inside the mouth 2-3 days after symptoms begin
Rash Phase:
- Appears 2-4 days after the first symptom(s).
- Usually begins as flat red spots appearing on the face, which then spread downward to the neck, trunk, arms, legs and feet.
- Small, raised bumps may also appear on top of the flat red spots.
- A fever may spike to more than 104 degrees Fahrenheit when the rash appears.
- Rash usually lasts 5-6 days
Source: National Center for Immunization and Respiratory Diseases (2024). Measles (Rubeola) Clinical Diagnosis Fact Sheet. CDC. https://www.cdc.gov/measles/hcp/communication-resources/clinical-diagnosis-fact-sheet.html