Home » Supported Research » Intraoperative imaging of macular hole repair to predict visual function outcomes
Intraoperative imaging of macular hole repair to predict visual function outcomes
Title: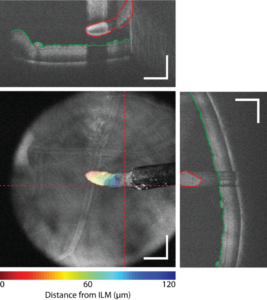
Intraoperative imaging of macular hole repair to predict visual function outcomes
Project Number:
1R01EY031769-01
Contact PI/Project Lead:
Yuankai Kenny Tao
Award Organization:
National Institutes of Health
Abstract:
Low vision and blindness affect over 40 million Americans and have an estimated annual cost of $25 billion for clinical diagnosis and treatment. The prevalence of visual impairment in adults 40 years and older in the United States is above 3.5% and expected to increase markedly due to population aging. Many ocular diseases are progressive and require surgical management at advanced stages, which involves precision manipulation of delicate semi-transparent structures in the eye. Optical coherence tomography (OCT) has revolutionized ophthalmic imaging by allowing for high-resolution noninvasive visualization of retinal microstructure and has become the “gold standard” for clinical diagnostics. However, despite broad adoption of preoperative OCT for surgical planning and predicting outcomes, postoperative functional outcomes may be highly variable. In macular hole (MH) surgery, ~90% of patients achieve hole closure and anatomic normalization but as low as 27% of patients achieve a best-corrected visual acuity of >20/40 (legal driving limit). We hypothesize that (1) structural changes in the retina during MH repair, which are prognostic of postoperative visual function, result directly from surgical intervention; (2) iOCT imaging of MH dynamics during surgery will enable quantification of image-based biomarkers and identification of corresponding tissue-instrument interactions that lead to poor functional outcomes; and (3) understanding the causal relationship between surgical manipulation and postoperative vision will benefit clinical decision-making and novel surgical technique and intraoperative feedback mechanism development for MH repair and other ocular diseases. Our collaborative program of engineers and clinicians will perform foundational imaging studies to understand the casual effects that surgical maneuvers have on postoperative vision recovery during MH repair. To overcome limitations of current-generation iOCT systems, we have developed multimodal spectrally encoded coherence tomography and reflectometry (SECTR) technologies that allows for simultaneous and intrinsically co-registered en face reflectance and cross-sectional OCT imaging. SECTR uses concurrently acquired spectrally encoded reflectance (SER) en face and OCT cross- sectional images to provide complementary spatial information in orthogonal dimensions and enable volumetric registration and tracking. Segmentation of motion-corrected 4D OCT datasets in post-processing has enabled retinal layer identification and quantification of tissue deformations resulting from surgical manipulation. Automated tracking and 4D imaging of MH dynamics (AIM 1) provides unprecedent data on structural changes resulting from surgical manipulation that have been shown to be predictive of postoperative functional outcomes (AIM 2). In vivo iSECTR imaging during MH repair will be performed to understand the causal relationship between surgical dynamics and postoperative visual function (AIM 3) and may lead to novel image-guided surgical maneuvers. Technologies developed during this project will have broad applications in personalized surgery, predicting outcomes, and image-guided feedback in a wide-range of surgical specialties.